Hackernews linked to a Medium post on ultrasound devices today, entitled "Why are Ultrasound Machines So Expensive?" which, being my core area of expertise with over 20 years in the industry, I was interested to read. Sadly it fell into the category of posts by someone with training in one area, which leads to an overconfidence of knowledge over what happens in another area, a lack of appreciation for the complexity and difficulty of the jobs of others, and as a result misses many of the subtleties (or not so subtleties) of an intensely difficult technical field.
The premise of the article is "Why is even a cheap ultrasound system over $30,000 when I can buy the bits and pieces for next to nothing and it's really easy to make? It's not that hard, I looked into it for a couple of hours!". While a premium ultrasound system with transducers can be $150,000 or more (a fraction of the price of CT and MRI systems) it's the most common medical imaging modality in the world for a reason - so allow me to refute this position that it's simple and overpriced.
What's my knowledge in this area to be able to comment? My Ph.D. was in the modelling, design, construction, and testing of this type of device. For 13 years I led a consulting group that produced the industry standard modeling software for ultrasound, and participated in and led many projects that designed and built ultrasound devices for a wide variety of industries, including medical. I am the Associate Editor in Chief of the IEEE Transactions on Ultrasonics, Ferroelectrics, and Frequency Control, the leading peer-reviewed journal for this subject, and chaired the IEEE Ultrasound Technical Program Committee for Transducers. I have worked in some of the largest medical ultrasound suppliers in the world, and worked with some of the smaller ones too. I've built and delivered commercial software critical for a business, around the world, and supported it for years. There's not many people with my background to evaluate the technical from both the hardware and the software side of things.
FYI, what I'm writing here is generic information, and not tied to any one company in particular, so there's nothing proprietary in what I'm about to say. Those of you wanting to learn more yourselves, I highly recommend Tom Szabo's book "Diagnostic Ultrasound Imaging: Inside Out" for a readable, and broad, coverage of the topic.
Let me start with demolishing this argument in one really quick paragraph citing not anything technical but Economics 101. If you can really build an effective ultrasound system that people want to buy for significantly less than the currently available price when you've no expertise in the field, then why hasn't someone else with vast experience in the field gone and done exactly that? Or why hasn't one of the major companies massively dropped their prices to corner the market? If there's collusion between the companies to fix prices, why hasn't a government somewhere sued them (and believe me, from being inside these companies, they are paranoid about playing by the rules and not accepting kickbacks or doing anything seen as fraudulent). I'll cover the FDA and regulatory later, but for now take my word that while it's a part of the cost, it's not the majority, and seriously, you don't want to use these things without strong safety regulations.
Next, let me cover that I've built hardware and software, and as difficult as software is, hardware is harder. If you make a mistake in developing hardware, you don't recompile the fix to get a new product in an hour, you rework and then rebuild taking weeks or months sometimes. With hardware you have to ship a product that works, you don't get to fix it in the field with an update, you don't get to ship with an EULA or a warranty that says "as-is", and you have to support the same product in the field sometimes for decades. With software you can develop your product in a small room with a laptop, but the tools to build hardware can be expensive and large with high running costs. Software also doesn't have suppliers who change materials, formulations, prices, or even go out of business and leaving you at a loss for components. If you want to mitigate all those risks for hardware compared to software, you need people to do so, and they cost money.
Now having said that, on to the technical. An Ultrasound System is made up of three major components - the transducer, the system, and the software. The transducer is what you hold in your hand, contacts the patient, and transmits and receives the ultrasound. There are multiple available transducers for every system, each with its own application, so a system has to support a potentially wide range of transducers.
The transducer is connected via a cable to the system, which has all the electronics to receive the signals and convert to an image to be displayed, and allow the sonographer to change settings etc. The software runs on the system, and allows for the display of the image, though these days the lines between where the hardware and software boundaries for imaging are, are getting blurred somewhat. In hospitals it's usually a cart, but there are some more compact (and more limited) systems available.
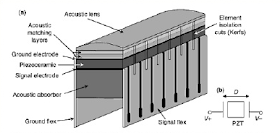
Let's take the transducer (some of these images are taken from this presentation, or here, which are good intros)
Starting from the top, you've got the lens (the bit that contacts the patient). This has to perform a certain amount of focussing of the ultrasound, and attenuate the signal enough you don't get reverberations at the skinline and obscure the image, but not so much you lose too much signal. It's got to ensure good contact with the patient, thick enough to be part of the insulation, and robust enough to be cleaned/disinfected as well as dropped and mistreated over the years of lifetime. Thickness has to be consistent across the surface, if you shift too much of a % of a wavelength over the surface then you'll distort the image. And remember ultrasound wavelengths are usually on the 100 micron order. But that's simple, right?
Then we have the matching layer, designed to ensure coupling ultrasound from the high acoustic impedance piezoelectric to the low impedance body. These days it's usually more than one, and each has to be a specific thickness, density, stiffness, and attenuation. Sometimes you need them conductive, and sometimes insulating. They also need to be machinable (diced, see below), and constant thickness, just like the lens above.
Then we come to the piezoelectrically active material - this is what converts electricity to vibration, and vice versa. Again it has to be a specific thickness, and consistent across the surface to a level you measure in microns. Which material you use is important, the cheap stuff is variable and lower performing, the stuff that's specced tightly and performs well is expensive. It has to not depole (lose its piezoelectric effect) at temperatures you run the probe, and withstand high electric fields across it. Piezoceramic like PZT has been the staple for years, but these days, to support the advanced imaging modes demanded, it can be single crystal piezoelectrics, which are more expensive, higher performing, but harder to work with. PVDF, sputtered materials, and the cheap PZT you make buzzers with are essentially useless for this type of work, despite being 'piezoelectric'.
Then there's the backer, a material that absorbs just the right amount of acoustic energy, so that you get a short pulse coming out the front that can image, but not so much that it reduces the signal to an amplitude too small to work. It's also in the thermal path, usually can't be electrically conductive, and not so large that the sonographer notices the weight.
Next you have to bond them all together, make sure they stick. The bondline has to be thin enough that it does not disturb the acoustic path, but not so thin that there is delamination and it's not a robust device. That means micron bonds, consistently across the surface. Easy, right?
Now you've got your acoustic stack. OK, now you can dice it - cut it into the elements that generate the image. Yes, you have to make many elements to make an image - in most transducers there are around 100 to 200 elements, left to right, across. A device with 20 elements, as the Medium article posited, are useless for any serious imaging application. You have to cut through all those matching layers and piezoelectric, electrically and mechanically isolating each from the neighbour, but not breaking the thin sections you leave, while making them thin enough that grating lobes and other artifacts don't spoil your image.
Then you have the flex circuit, to take the signal to and from each element, and it's got to be precisely aligned with the elements, that's on the 100 micron order to position (yes, each element is around the width of a human hair or two), and then it's got to connect to the cables off to the system - all 100 to 200 wires down a cable that's a couple meters long, and thin/light enough for someone to use 8 hours a day without getting repetitive strain injuries. Do you know how thin that makes each wire? Try calling a few cable vendors and ask for a small diameter cable with 200+ connectors that will actually conduct a signal without significant crosstalk and let's see where you end up on price.
Finally, you have to put it into a housing that's ergonomic for the sonographer to use, large enough to hold the acoustics, small enough not to be heavy, and not sharp to hurt the patient. On top of that it also has to be designed so that it doesn't get so hot it burns the patient or the medic.
Simple!
Right. And that's the most basic version. I haven't gone into multi-row probes, those on a curved backer, exotic materials, those with electronics in the handle, what the dimensions of each section have to be to give the right acoustics, steering, spectral response, thermal characteristics, electrical impedance to match to the system, or all the other difficult things that in reality you have to deal with if you build and sell these devices.
Oh, and I forgot about consistency, reliability and cost. These devices have to last for years, be close enough in consistency from device to device the system can image with them and the user doesn't know the difference, and be low enough cost that the user will buy them and the company makes a profit. Ever made a protoype? Ever made 2 of them? 4? 100? 10,000? And made them all the same? Yep, it's a different world when you have to start selling and supporting products.
Ooops, I forgot, and testing to meet your own internal specs as well as those of the FDA and other regulatory agencies, to make sure that these devices don't electrocute or burn you, and give the right medical data so that you aren't misdiagnosed and receive the right treatment.
And I haven't even got to the system or software yet (I'll try to get to a part II on that). Just the transducer requires people with knowledge of acoustics, imaging, clinical need, materials, mechanical design, electronics, thermal, processing, regulatory, safety, chemical compatibility, user experience, reliability, QA, business, and a whole host of things I just don't have room to list. Then you need the support staff, the building, HR, admin.
This takes a huge amount of expertise and effort - almost as if some people's lives depend on it.
This takes a huge amount of expertise and effort - almost as if some people's lives depend on it.
I've got a lot of experience designing and building these things. Could I setup a company to do it, and do it well? Yes. Could I do it significantly cheaper than others do it right now? Nope.
Put that all together, and you have an incredibly complex electromechanical product with components on the micron scale, that has to work reliably in the field for years, reproducible across all that are made without the benefit of mass volumes (no millions of devices here), upon which medical decisions that lives can depend are made - and that's just the transducer - so you need to ask "Why are medical ultrasound systems so inexpensive?"



The 200 line cable seems like a mistake. Why not embed DACs and a DSP in the sensor and run the data over a USB cable? I suspect that there just isn't enough demand to allow economies of scale yet...but that will change.
ReplyDeleteNot a mistake - electronics require power, generate heat, and cost. There are limits to physical size and weight you can go to, and strict limits (both practical and regulatory) on heat. Electronics can't shrink to the smallest process nodes due to high voltages required. Remember you have up to ~200 channels each needing to be sampled sufficiently to represent a multi-MHz signal.
DeleteThere are more transducers that use electronics in the handle being built in recent years, especially the transducers that are 2D, as there you are into 1000's of elements, but they are also substantially more complex to build and pricier.
As Paul said, but with a bit more. At 7 MHz, 200 channels, 10-bits (I'm being generous, it's probably more), Nyquist requires ~15 MSPS per channel, or 150 Mbps per channel at 10-bits.
DeleteDoesn't seem so bad right? I mean, it's ~1/3rd (in reality, close to an entire due to other factors) of a USB2.0, and less than 2-3% of a USB3.0 or thunderbolt.
But wait, 200 channels...ok, so we are at 30 Gbps, which is sporty for any transport.
And then on the ADC side. Let's say there are 150MSPS/10-bit ADC's that consume as little as 50mW, well, now we have 10W of power just to run the ADC's, all in the wand, plus the data transceivers, plus the power amps for the transducers, plus the DACs to drive them.
As Paul alluded to, there is such a market here where if it were even _possible_ to gain competitive advantage by further integration ofhe up/downstream electronics into the wand, it would have been done.
That said, as the need for dense, many channel, beamforming/amplifier/ADC/DAC silicon is driven by mobile consumer devices, it may be possible to do exactly this at some point in the near future, at which, I'll bet you see thighs change dramatically on the electronics side. However, the transducer aspects of cost and complexity will likely remain the same and slowly evolve cheaper, rather than having a paradigm shift.
So TLDR; ultrasound equipment are expensive because they don't have the economies of scale of say, smartphones (or even low end digital oscilloscopes)?
ReplyDeleteThis comment has been removed by the author.
DeleteI think that misses the part where he describes the sensors are also incredibly difficult to manufacture or that the cables are horrendously expensive.
DeletePartly, but not completely so. You don't have the same number of channels on a scope, for example. Reread the post about all the constraints just for a probe (and you need several different models of probes)
ReplyDeleteYou have a fine point, hardware is really hard, medical hardware - especially so. The medium blogpost you replied sure feels lightweight.
ReplyDeleteBut how can you be so sure that MEMS/CMOS integrated technology won't replace traditional mechanical transducer technology? Look at accelerometers/gyros - they are all MEMS now, a couple dollars per unit. Compare that to old mechanical precision gyroscopes and their prices.
Looks like even some military missles started to use MEMS IMUs nowadays: http://www.systron.com/applications/defense/inertial-sensors-missile-guidance-control
There is at least one research paper [1] demonstrating integrated MEMS ultrasound transducer+pulser+amplifier+ADC combo. If such device could be scaled channel-wise and mass-produced (which happened for MEMS IMUs), it could serve as a basis for low-cost portable ultrasound. With most of the transducer being a single solid-state device, what is left is acoustic lens, enclosure, high-performance DSP system (could be a custom 28nm|14nm|10nm ASIC - even high end GPUs embedded in mobile SoCs can handle up to 500 GFLOPS nowadays) and the software.
(on a sidenote: Looks like this is similar to the approach Butterfly Network is pursuing.)
Even if we don't venture into unproven technology, a transducer could be bought for 1000$, and there are already fully integrated transceiver frontends (see https://www.maximintegrated.com/en/products/analog/data-converters/analog-front-end-ics/MAX2082.html , it is a 8 channel IC that costs 6000$/unit, but it is certainly 10x+ overpriced because similar amp+ADC parts from Ti cost mere 100$ http://www.ti.com/lsds/ti/data-converters/ultrasound-products.page ), so looks like 96-channel analog frontend could be bought for another 1000$. Digital data acquisition and processing could be done in 300$ Xilinx Artix 7 FPGA https://octopart.com/xc7a200t-1ffg1156i-xilinx-27810763 , final postprocessing and output could be done with 200$ snapdragon 821 SoC (though one coud ditch the SoC and buy FPGA with built-in CPU IPs, or, in theory, one could do a lot of DSP on 821's openCL compatible 500 GFLOPS gpu).
Looks like with enough NRE costs 3000$ portable ultrasound device is not impossible.
If creating a low-cost portable ultrasound device is technically possible, isn't it a moral thing to realize this opportunity?
Billions of people are too poor to afford these services/devices at current prices, you know.
1. https://www.ncbi.nlm.nih.gov/pubmed/23853268
I've tried to reply to many of your points in my latest post, thanks for taking the time to ask some detailed questions.
DeleteEveryone working in ultrasound engineering wants to produce devices that work for as many people as possible. There are lower cost systems out there, but can they deliver a needed quality at a price point that's affordable? It's not as easy as you list above, but the technology is getting there, and I expect to see more lower end systems with limited uses in the next few years. In 20 years, it could be a completely different market, though the high end might be adding some amazing new modalities in that time. Hardware might get down to a lower cost, but quality software and systems support still costs so consumer level prices will be difficult/impossible until volumes grow drastically (bit of a chicken and egg thing there).
If you want to get involved in trying to make that a reality, there are companies that will hire talented people!
BTW I'm familiar with that reference and that group, they do good work - however that performance still doesn't begin to match the highest end requirements for ultrasound, but it's a step along the way.
First of all, thanks to everyone for their comments.
ReplyDeleteThis ended up as a thread of its own on HackerNews again, so I'll be writing a more detailed response to what people have written here and in HN as a post in itself for later today (I hope).
https://news.ycombinator.com/item?id=13241295
What are your thoughts on this product by Phillip's
ReplyDeletehttps://www.lumify.philips.com/web/
Matt, I started to reply, but decided to do a separate post to address my opinion of this and similar devices. It should be up shortly.
DeleteThank-you Paul! Great piece for the masses (me). We really appreciate the experts that invest their time in the rest of us and those that pose the questions that incite the responses. Merry Christmas!
ReplyDeleteYou're welcome, and I appreciate everyone who takes the time to ask questions. Merry Christmas to you all too.
DeleteThis comment has been removed by a blog administrator.
ReplyDeleteThis comment has been removed by a blog administrator.
ReplyDeleteThis comment has been removed by a blog administrator.
ReplyDeleteas a medical doctor with bit technical knowledge trying to understans the working
ReplyDeletenice post.thanks.
i got here through the linked article at the top and to be fair, author was rather thinking about making some DIY ultrasound for educational purposes if i got him correctly.
ReplyDeleteit sure isn't highend ultrasound with 3d imaging and it's rather intended for africa,but he linked one really interesting project with aim for £30-40 pricetag, with single transducer element a not bad images(unusable for heart though)
http://www.ncl.ac.uk/eee/research/coms2ip/sensors/ultrasound-imaging/
This comment has been removed by a blog administrator.
ReplyDeleteThis comment has been removed by a blog administrator.
ReplyDeleteThis comment has been removed by a blog administrator.
ReplyDeleteThis comment has been removed by a blog administrator.
ReplyDeleteThis comment has been removed by a blog administrator.
ReplyDeleteHi,
ReplyDeleteWould it be possible to get in touch? I'm a PhD student at UCL working on a spin-out from my research which is aimed (partially) at the low-cost ultrasound market. It uses a fundamentally different approach to PZT or even CMUT. I'm working closely with the biomedical ultrasound and the photonics groups here. I recently presented some early results at IUS 2018 in Kobe. Would be great to hear from you.
Best wishes,
Tom
thomas[fullstop]robbins[fullstop]15@ucl.ac.uk